Authors: Shreekanta Kumar Sahu, Sr. Consultant, CitiusTech and Dr. Vishal Anand, Sr Business Healthcare Analyst, CitiusTech
Value-based care and healthcare consumerism have taken a front seat in healthcare, becoming a business imperative for health plans and payviders to transform and grow digitally in their efforts to introduce new products and compete for market share.
In the previous blog of our payvider value chain series, we discussed the importance of performance management for payviders. This blog discusses the role of data science and digital innovation for payviders.
Payvider Digital Transformation Objectives
The current wave of digital transformation has been significantly accelerated out of necessity during the pandemic. Forced innovation has created an opportunity for payvider organizations. Evolving and sophisticated technologies enable payviders to create a strong foundation across their three most important stakeholders by creating meaningful member, provider, and broker relationships.
Successful stakeholder relationships rely upon timely, accurate, and accessible data and analysis; streamlined business processes and operations; as well as useful and engaging digital tools and experiences.
Creating a robust and scalable foundation for digital transformation goes beyond “member experience” to address many business and care issues -- improve outcomes, reduce administrative and medical costs, increase revenues and profitability
Key Digital Transformation Goals
Improve member experience throughout the journey: Advanced technology and tools within data science, artificial intelligence (AI), and machine language (ML) equip payviders to proactively engage members in selecting the right health plan product, address member concerns, answer member queries, help members achieve health and wellness goals, and identify risks and gaps in care. While payviders have traditionally lagged in this area, technology and expertise is accessible to leverage these tremendous opportunities.
Administrative simplification and cost reduction: Payviders want to streamline and squeeze waste out of administrative functions like claim processing, provider data management and directory, benefit management, care management, credentialing, and network management. Beyond administration, optimizing resources through medical services can be achieved by adopting or solidifying digital health offerings like telehealth, remote patient monitoring, personalized care, and wellness-preventive care.
Create or scale new revenue streams and grow overall revenues: Focus on developing new digitally-enabled products for specific market segments, establishing analytics-driven benefit plan design, and using advanced data analysis and automation to empower and simplifying sales and enrollment process adds resilience and stability to the payvider model.
Breaking Down Payvider Digital Strategies
- Enhancing Member Engagement
Members are seeking a more personalized approach, transparency in treatment cost, advocacy and navigation support for chronic illness, and benefits that meet their varied lifestyles and goals. Deeper member engagement through connected digital health tools impact and influence member behavior, inspire members to take proactive control of their health and wellness, which can lead to reduced cost and greater member loyalty and positive word-of-mouth.
Proactive Care Management & Wellness
Predictive analytics and comprehensive care management act as glue that holds together every value-based care program. The prevention of diseases and illness is a major focus of payviders as they move away from fee-for-service, encounter-based care models. Yet, they often find themselves adding traditional, non-billable services to their care management repertoires in an effort to get ahead of chronic diseases and deliver comprehensive care.
Visibility into patient outcomes is critical, requiring organizations to invest in predictive analytics tools that meld clinical, health, and financial data with newer sources of insight like social determinants, community data, and member-generated data.
Predictive analytics uses modelling, data mining, and statistics, coupled with AI/ML to evaluate historical and real-time data and create probabilistic assessments. These predictions offer a unique opportunity to identify potential trends at the individual and population level. Beyond improving patient health and lowering costs, proactive modeling enables care managers to take an integrated approach that’s aligned with the shift to value-based, holistic care.
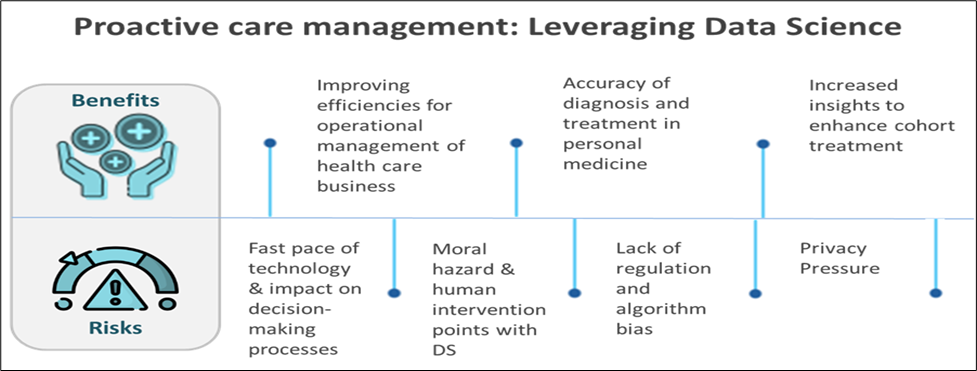
Figure 1: Benefits and risks to leveraging data science for proactive care management.
Virtual Care, Telehealth and Remote Patient Monitoring
The explosive growth of everything tele- and virtual since the pandemic began has been remarkable. For payviders, it’s time to create a strategy that establishes where all of these engagement and care channels fit for the longer term.
The benefits for payviders are many, but should be weighed against cost when considering value gained during the pandemic and ongoing importance to new business and market plans.
Access: Virtual visits empower people to confer with their caregivers from the comfort of their own home. And it isn’t just about comfort. In rural areas, the ratio of patients to primary care physicians is less than 40 doctors for every 100,000 people. In these areas, virtual care offers not just convenience but actual access to caregivers that patients wouldn’t otherwise experience.
Continuity and decreased risk: Virtual care can cut the prevalence of no-shows, saving time for providers and cutting costs for the organizations that employ them, improving quality and preventing costly downstream events like hospital admissions and readmissions.
Medical Internet of Things (MIoT): Real-time remote monitoring for patients living with chronic diseases or who need continual medical attention, also reduces health risks and possible exacerbations, reducing hospitalization and providing timely medical intervention based on real-time patient data.
Personalized Member Experience
We believe that successfully enhancing the members’ digital journey relies on knowing their preferences and having the data and tools to deliver those experiences. Next-generation member engagement tools empower members to make high-value care decisions while enable health insurers to improve care quality, increase member satisfaction, and reduce medical spending.
Health plans including payviders are leveraging digital technologies, advanced analytics, and personalization capabilities to create more effective digital support tools and scale member engagement solutions already available.
Data science and advanced analytics are foundational to all aspects of next-generation member engagement, particularly when supporting a member during critical moments in their care journey.
- Advanced analytics helps digital teams develop actionable personas to identify member segments with distinct features and preferences
- Real-time signal interpretation makes it possible to track member behavior and enables rapid multivariate testing of different member experiences
- Episode analytics identifies and reveals highly-granular sources of value
- Enhanced services like proactive care management; triggers that engage social work; and admission, discharge, or transfer (ADT) alerts add value to the patient experience while helping providers stay on top of their high-risk populations
- Streamlining Operations to Improve Quality and Lower Cost
Streamlining operations by using analytics and automation supports payviders to improve the quality of care and reduce costs. This puts payvider in a strong position to achieve greater customer satisfaction and improve the bottom line.
Claims Management and Analytics
Automation using AI/ML and robotic process automation (RPA) can improve auto-adjudication rates. This reduces manual intervention thereby reducing error and cost. AI/ML can be used to scrutinize claims to detect clinical edits and fraudulent claims at the pre-processing stage, as well as proactively suggest decisions before the claim is paid. This can reduce the time spent on “pay and chase” tasks, considerably.
Also, claims data are a great input for predictive analytics. Member claims history gives diagnostic, lab results, and demographic indicators and warning. Predictive analytics can detect conditional risks before diagnosis and alert for early intervention. Additionally, using predictive analytics to perform volume forecasting and categorizing incoming claims helps payviders manage resources, budget, and inventory.
Chatbots & Virtual Assistants
- Claim agents: Processing a claim manually requires claim agents have access to multiple applications for critical information. This process is very time consuming and prone to error. VAs can access the required information more accurately and efficiently.
- Customer care agents: These VAs can answer hundreds of queries from members and providers by accessing multiple applications and providing answers to different types of queries.
- Member portal: A VA can streamline data queries, delivering member information like claim status, coverage and benefits information, limits and accumulators, and provider search to name a few. Fewer clicks and time spent on portal can translate into high member satisfaction with digital tools.
- Provider portal: Members use portal to get verity of information that includes, Claim Status, Member eligibility, Appeal status, Coverage information etc. With help VA, the number if clicks and time spent on portal can be reduced.
- Sales portal: Help small business/Individuals in selecting right benefit plans based on member demographic, risk status, and cost etc.
Benefit Plan Design
Integrated data analytics supports informed decision-making on benefit plan design. Addressing the health needs and member expectations of a fast-changing demographic requires a range of products tailored to population segments. Robust capabilities for risk stratification and predictive analytics of medical cost are critical to fiscally-responsible and market-appropriate plan design. Analytics can forecast potential savings on proposed benefit plan changes and calculate the potential effect of various wellness program options that might be embedded within the plan. AI/ML analytics solutions are appropriate to help payviders select the best plan based on risk and cost variables.
Designing specialized medical benefits can reduce clinical and administrative costs for more complex and chronic medical conditions, reducing the cost of care, managing organizational risk, and improving outcomes for members who face complex health scenarios and disease like organ transplant, cancer, kidney disease, heart disease, and musculoskeletal conditions.
Population Health Management (PHM)
PHM relies heavily on clinical and claims data as part of benefit design and delivering timely and appropriate care and interventions. As more clinical, financial, social, and patient-generated health data is available digitally, aggregating and transforming these data and applying analytics is becoming increasingly required for scaling PHM.
Because payviders must aggregate and analyze data on specific populations to derive insights and evidence, developing advanced analytics and using data mining are needed to recognize common risks across cohorts, devise strategies to address them, and implement programs to improving outcomes.
Identifying New & Increasing Risks and Care Gaps
Because payviders have limited proactive recognition of which members will have gaps in their care, they have developed sophisticated capabilities to recognize those gaps but they are, many times, addressing them after the fact. Using social determinants of health, in addition to historical claims data, adds an innovative layer to program design and targeted outreach initiatives.
Performing member risk identification and stratification to optimize health intervention requires a lot of varied data, and a robust enterprise data warehouse can aggregate data from internal claims and clinical systems and from external systems to achieve a higher level of risk ID and stratification accuracy and volume.
Provider Data Management
One constant challenge that payviders face is maintaining accurate, up-to-date provider data. Provider data like address, affiliation, license, and sanctions change frequently and require multiple external sources. Aggregating, matching, reconciling, and merging disparate data into a single source of truth is key.
Advanced technologies like blockchain enable seamless and auditable data integration, reconciliation, and validation. These data management technologies deliver short-term and long-term benefits, including easier access yet better data security, improved directory data quality, streamlined compliance, and reduced maintenance and transaction costs.
Scalable Automation
Increasing costs and dwindling profitability pressurize payvider organizations, limiting their ability to reinvest and scale growth. While most payer organizations, including payviders, have tried to reduce operational burdens and cost using RPA, savings have been limited to individual business functions, processes, or lines of business. Adopting enterprise -level automation will continue to be a strategy for business efficiency and profitability with the goal of reducing cycle time for repetitive and time-consuming manual tasks, eliminating potential bottle necks, and reducing costly human errors.
Multiple intelligent automation technologies can achieve these goals:
- RPA creates a digital workforce, improving performance of standardized manual tasks
- AI/ML embeds intelligence into standard processes and reduces dependencies on overburdened resources
- Natural Language Processing (NLP) can act as an interface between humans and machines, converting standard speech and text into structured information and documents
Leveraging automation in small pockets within the organization may be a good starter strategy, however automation is demonstrating immediate ROI for healthcare organizations. Achieving automation at scale requires a holistic approach and a comprehensive strategy, which maximizes the value of each technology for enterprise and targeted business and task-related objectives.
In summary, payviders have a unique opportunity ahead of them. Taking a holistic approach to business transformation and leveraging the right digital technologies to achieve that requires sophisticated data science capabilities, artificial intelligence, appropriate digital tools, and intelligent automation. These are the keys to market and member success.