Shobhit Saran, AVP Health Plans & Aritra Roy, Sr. Healthcare Business Analyst, FAST+
On 10th December 2020, CMS proposed a new set of rules to further enhance healthcare data interoperability between payers, members, and providers. While payers continue to work on building an infrastructure to comply with CMS’ interoperability and patient access final rule, these new rules aim to reinforce the positive impact of earlier rules.
The new proposed rules focus on the prior authorization workflow to enhance patient safety and minimize healthcare services and costs. Although a crucial and effective utilization management practice, Prior Auth management is often challenging. Healthcare providers spend an average of 20 hours per week on Prior Auth activities as they are unsure about
- Medical procedures that may (or may not) require prior authorization
- Types of information to be shared with payers for approval
- Payer communication – what information must be shared with payers
Most Payers and Providers have established processes of enabling prior auth workflow that often results in administrative burden, physician abrasion, and poor patient experience.
CMS’ proposed rules aim to overcome these challenges by standardizing and streamlining this process. The proposed rules will apply to payers in Medicaid, the Children’s Health Insurance Program, and qualified health plans.
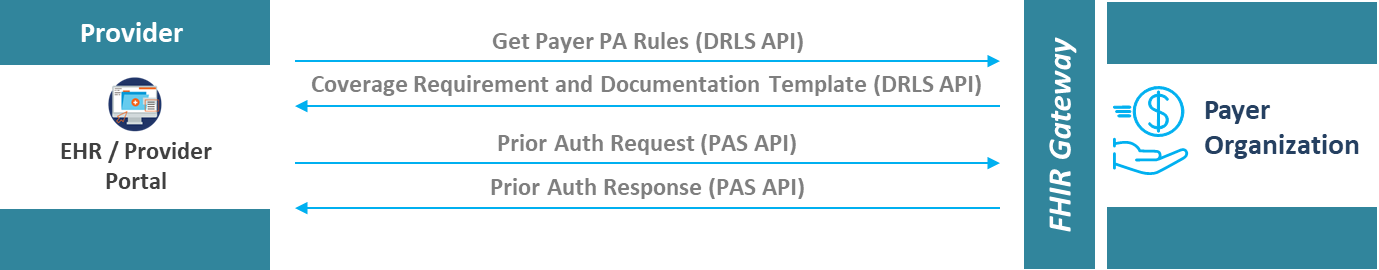
Payers are encouraged to build and maintain an HL7 FHIR-enabled Prior Authorization Support (PAS) API, that would enable providers to send prior authorization requests and receive responses electronically, directly from the provider's EHR or other systems. Essentially, a provider can call a payer’s PAS API to send prior auth request to the payer, and the payer should ingest that FHIR data using a FHIR parser, perform utilization review on that information and send a FHIR-based response back to that provider.
Under the proposed rules, payers are also required to build and implement an additional Document Requirement Lookup Service (DRLS) API for providers to anticipate any documentation would be needed for which treatment by the particular payer. This rule draws inspiration from the Da Vinci Prior Auth use cases and has even proposed conformance to the Implementation Guidelines (IG) of Da Vinci Coverage Requirements Discovery (CRD) and Da Vinci Documentation Templates and Rules (DTR) use cases. The DRLS API is proposed to be populated with a list of covered items and services for which prior authorization is requested, along with correct mention and description of the documentations required for Prior Auth submission.
In the prosed rules, CMS highlights that payers will need to provide specific reasons for any denial, consequently governing transparency in the system. To promote accountability, the rule also requires payers to make public certain metrics that demonstrate how many procedures they are authorizing. One of the several new rules also mandates shortening the prior authorization window to 72 hours for urgent requests and seven calendar days for standard requests.
In addition to the above rules, CMS has also proposed that payers should share pending and active prior auth data requested by members and providers using FHIR-based Patient Access API and Provider Access API respectively. Pending and active prior auth data are also proposed to be shared as part of Payer-to-Payer data exchange to minimize duplication of authorization when members switch health plans.
The prior authorization policies are proposed to take effect from January 1, 2023, with the initial set of metrics proposed to be reported by March 31, 2023.
CMS understands the importance of seamless information sharing and is focused in fulfilling provisions of the 21st Century Cures Act. The proposed rule is a welcome step towards improving patient care and health outcomes.